Oesophageal Cancer
In addition to surgical procedures, irradiation plays an important role in treatment. Esophageal tumors are irradiated preoperatively or without a surgery if this is not possible for any reason. In conventional photon irradiation, it is very problematic to capture the entire irradiated area without a significant radiation dose to the lungs and liver. In contrast, the required dose in proton radiotherapy can be easily delivered to all the necessary areas and the curative effect can be achieved at significantly lower risk.
Suitability for proton therapy is tied to the exact location of the tumour in the esophagus.
Hepatocellular Carcinoma (HCC)
Proton irradiation has been applied in the treatment of HCC for over 20 years. The most experience comes from Japan, followed by the USA. The number of treated patients has already reached thousands and the number of printed publications is more than one hundred (Phase III or Phase II studies).
- Effectiveness of proton therapy is similar to surgery in terms of survival parameters, i.e. 2nd most effective modality after transplantation.
- Very favorable toxicity profile.
- Fractionation regimens are variable and can be adapted to different needs.
Pancreatic Cancer
Click here to learn more about pancreatic cancer.
Contraindications for Proton Radiotherapy
- Metastasis (the cancer has spread from its primary location to other organs)
- Metal/ceramic parts in the radiation field
- Presence of a pacemaker
PROTON IRRADIATION
PHOTON IRRADIATION
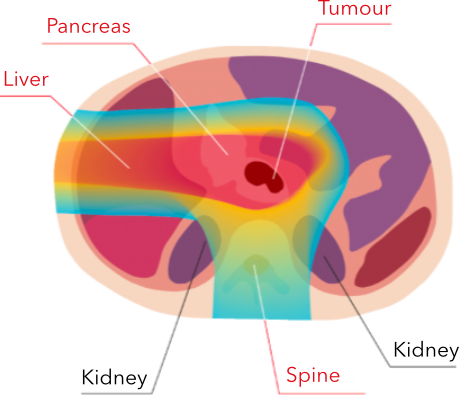
Protons target the tumour directly, sparing healthy tissues and organs from unwanted effects.
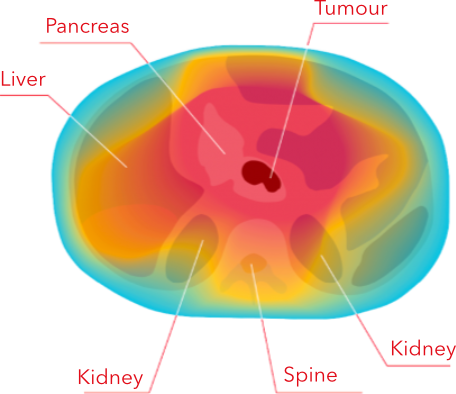
Photons irradiate the tumour as well as the healthy tissues and organs around it.
For irradiated volumes in the upper abdominal cavity, i.e. in the treatment of pancreatic or hepatic tumors, compared to standard radiotherapy, proton radiotherapy:
- reduces the dose to the abdominal cavity, in particular to the small intestinal loops. This reduces the severity of acute undesirable effects of radiation, such as nausea and diarrhea. Higher doses of radiation can also be used to achieve a greater antitumor effect (dose escalation)
- reduces the dose to the kidneys, which ultimately leads to a decreased likelihood of nephrosclerosis (renal vascular disease) and renal hypertension (increased blood pressure resulting from renal involvement)
- reduces the dose to the liver tissue, thus reducing the risk of hepatic failure
For irradiated volumes reaching into the chest cavity, such as in the treatment of esophageal cancer, compared to standard radiotherapy, proton radiotherapy:
- reduces the mean dose to the pulmonary tissue, thus reducing the risk of developing inflammatory lung disease (pneumonitis)
- reduces the dose to the heart valves, coronary arteries and heart muscle. This reduces the risk of early ischemic heart disease, valve defects and heart muscle disease (cardiomyopathy)
Proton therapy can be used to deliver a sufficiently high and effective dose of radiation to the area affected by a tumor, with a tolerable radiation dose to the surrounding and vulnerable organs such as the liver, kidneys, stomach, duodenum, small intestine and spinal cord.
Proton therapy can also be used to deliver an effective dose to the area of regional lymph nodes, which are also often affected by cancer.
To learn more about proton therapy for gastrointestinal cancer, or to find out if you are a suitable candidate for treatment at our centre, contact us today. Our team will get back to you with a detailed response as soon as possible.
* Suitability for treatment at our centre must be determined by our medical team.
